Free Shipping PAN India
Aveil Rejuveil is a sugar-free, vegetarian supplement with antioxidants, vitamins, and minerals that brighten skin, reduce pigmentation, support collagen, strengthen hair and nails, and boost overall wellness and vitality.



Aveil is an attempt to create breakthrough products which are a fine blend of organic and chemical free ingredients utilised in their best form.
It aims to create a range of skin care products which effectively heal and provide relief from skin conditions with least or no side effects.
Hear it directly from our customers who left these reviews on Amazon.
Aveil uses safe, simple, free of harmful chemicals ingredients that are expertly crafted to match users’ needs.
Next generation sunscreen with unique nano technology designed to protect our skin from not only UV light but also Infrared rays.
Vitamin C serum with Hyaluronic Acid and Tranexamic Acid to keep the skin hydrated, aids in skin repair and reduces inflammatory damage from day to day stress on the skin.
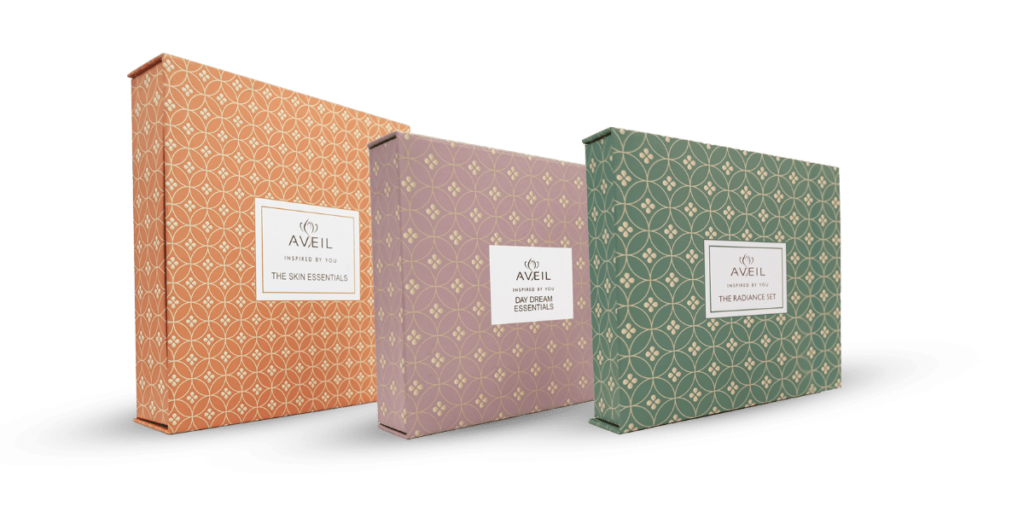
Make every occasion special with a box of Aveil Essentials. Choose any of our pre-made gift sets and put a smile on a skincare lover’s face.
Aveil’s apothecary consistently formulates new products and offers throughout the year to cater to your skin and wellness needs.
₹1,949 Original price was: ₹1,949.₹1,559Current price is: ₹1,559.
₹3,299 Original price was: ₹3,299.₹2,639Current price is: ₹2,639.
₹3,899 Original price was: ₹3,899.₹3,119Current price is: ₹3,119.
Aveil’s latest offers, combos and products on sale.
₹1,949 Original price was: ₹1,949.₹1,559Current price is: ₹1,559.
₹3,299 Original price was: ₹3,299.₹2,639Current price is: ₹2,639.
₹3,899 Original price was: ₹3,899.₹3,119Current price is: ₹3,119.
₹2,178 Original price was: ₹2,178.₹1,851Current price is: ₹1,851.
₹2,598 Original price was: ₹2,598.₹2,208Current price is: ₹2,208.
₹4,576 Original price was: ₹4,576.₹3,890Current price is: ₹3,890.
We love hearing from our customers. Connect with us on social media to share your feedback and thoughts.