Free Shipping PAN India
Eczema is a well-known dry, inflammatory skin condition. Although it is mainly seen as a problem in children, it can affect people of all ages. You may find that, even if you have ‘grown out’ of childhood eczema, it can come back when you are an adult. Although the exact cause of eczema is not known, your genetics play a role, so you may find it runs in your family.
What you might not realise is there are many different types of eczema that can affect different body parts. The good news is that eczema is not contagious, but you may have times when it is worse than others – this is known as a flare-up.
If you have eczema, your skin is different to the skin in healthy people. It may not produce as much fats and oils, which makes it harder to trap moisture in your skin. This weakens your skin barrier leading to dry, irritated, cracked skin. Eczema skin is more prone to irritation and allergic reactions, making your skin red and inflamed.
Eczema can be itchy, making you scratch – and further damaging your skin in the process. This itch-scratch cycle can then continue to make your eczema worse.
There are a number of different causes and types of eczema, but the most common are:
There is no single known cause for atopic eczema, which is also known as atopic dermatitis. This long-term inflammatory skin condition is often genetic, with around half of cases linked to a specific gene. It can also be caused by your immune system or can be triggered and made worse by factors in our environment like extreme temperatures, soap, detergent, pollen, animal dander, house-dust mites and rough clothing.
Symptoms can be mild, meaning patches of dry skin, occasional itching and maybe some redness. Moderate symptoms include patches of red, dry skin, frequent itching, which can cause the skin to thicken; all of which can result in disrupted sleep. In severe cases, large red areas develop, with dry skin that is always itchy and cracked, which may bleed or ooze. In severe eczema, the effects go beyond the skin; in children it can limit their ability to do everyday activities, affects their quality of life and can make it hard for them to sleep through every night.
Although it can affect any part of your body, atopic eczema is most common on your scalp and between your body creases like knees, elbows and armpits; in infants the face is also a common area that is affected. It usually starts in childhood, with up to 90% of cases in children under five years of age. Although 10-30% of children have atopic eczema, they often grow out of it – as only 2-10% of adults are affected. The condition is more common if you have asthma and/or hayfever.
Contact eczema, otherwise known as contact dermatitis, occurs when an irritant or allergen causes an inflammatory skin reaction.
Dyshidrotic eczema, also known as pompholyx eczema, usually affects your hands and feet. While the cause is unknown, it has been linked to contact eczema, stress, heat and sweating.
Symptoms start with an itching, burning, prickly feeling in the soles of your feet and/or palms of the hands. Extremely itchy watery blisters develop on the soles of your feet, palms of your hands and outside of your fingers that then group together to form large, weepy blisters. These can become infected, swollen, red and painful then red and cracked as they dry out. You might find you have blisters for around three to four weeks before they vanish of their own accord. The condition can even affect the skin around your nails, causing swelling. It’s more common in adults under 40 years of age, particularly women. Around half of people with dyshidrotic eczema also have atopic eczema or a family history of this condition.
You might find you only ever have one bout of dyshidrotic eczema in your life, though most people find it is a long-term problem with recurrent bouts.
Also known as discoid dermatitis or nummular eczema, this condition causes ‘coin-shaped’ (round or oval), extremely itchy, dull red patches on your skin. It’s not known exactly why we get it, but having dry skin seems to be a factor. Discoid eczema develops suddenly, appearing anywhere on your body, but usually on your arms, lower legs and/or trunk. One thing to be aware of is that body washes, moisturisers and other materials that touch the skin can make discoid eczema worse in some people.
This form of eczema can affect anyone at any age but is slightly more common in adults. If you’ve ever had atopic eczema, allergic contact dermatitis or eczema as a child, you are more likely to develop discoid eczema. Chronic alcoholism also increases your chances of developing discoid eczema. Unlike some other types of eczema, discoid eczema does not run in the family.
This form of eczema is found in the parts of the skin where there are lots of sebaceous (oily) glands, such as the scalp, face and centre of the chest. Also known as seborrhoeic dermatitis, it’s believed to be caused by an inflammatory reaction to the overgrowth of a yeast that lives normally on the skin called Pityrosporum ovale. There are two types of seborrhoeic eczema: one that affects adults and one that affects infants.
Your skin will be pale red and inflamed with greasy-looking white/yellow scale on top. In the skin folds, like your armpits or groin, your skin may look more glazed and you may not have any scales at all. Where your skin is more exposed, the scaliness is more obvious and yellow. Your skin may be itchy and, in severe cases, can even be painful.
Mild scalp seborrhoeic eczema causes flaking skin and is better known as dandruff. If the condition affects your face, you may develop red, scaly skin around your nose and cheeks. In rare cases, seborrhoeic eczema can spread and become more severe, affecting large parts of the body but is not contagious.
Seborrhoeic eczema can affect people of any age, though in children you probably know it better as ‘cradle cap’. Around 4% of the population have seborrhoeic eczema, with dandruff affecting up to half of all adults. It’s more common in men, particularly those around 30 years old. For women, the peak time of developing the condition it is around 40 years of age. If you have another skin condition called psoriasis, you may find you also have seborrhoeic eczema at the same time.
Varicose eczema is also known as stasis eczema, venous eczema or gravitational eczema. When the valves in our leg veins are weak and don’t work properly, blood doesn’t drain well and pressure in the leg veins builds up. Hot, brown, itchy speckled spots that can blister appear on your lower legs. Your skin can be dry, extremely itchy and even painful. In severe cases, your skin can be scaly, weepy and crusty. You might even find that varicose eczema triggers eczema in other parts of the body. It’s important to treat varicose eczema to stop the skin breaking and forming ulcers on the leg, which can be hard to heal.
The condition is more common if you get varicose veins, are middle-aged or older, female or overweight, have high blood pressure or have had conditions such as cellulitis, phlebitis or deep vein thrombosis in the past. Unlike some other types of eczema, varicose eczema does not run in the family.
Not everyone has the same symptoms or signs of eczema. It depends on the type.
The symptoms can range from mild to servere depending on the cause.
There may be a number of reasons for eczema to flare up. You may have a few the following symptoms:

Itchy skin can affect any part of the body. It causes the skin to be less effective as a natural barrier. It can be helped.

The outer layer of our skin is known as the epidermis. Normally, this helps trap water to keep our skin moist. Flaky skin can be caused by damage to the epidermis or some other disruption to our usual skin renewal process.

Temporary redness can come from embarrassment (blushing) or a menopausal hot flush Lasting redness can be due to a range of reasons including sunburn or a reaction to alcohol, as well various skin conditions.

Skin with eczema is more liable to become red and inflamed on contact with known on contact with known irritants or allergens. Inflamed skin can become red on lighter skin and darker brown, purple or grey on darker skin.
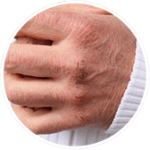
When the skin is dry, it can become rough and flaky. this can lead to small tears, or cracks in the skin that may bleed and ooze in severe cases.

To help protect the outer layer of skin from losing water, the skin produces an oily substance called sebum. If the skin doesn’t have enough sebum it loses water and feels dry

Pompholyx is a type of eczema that causes tiny blisters to develop. It usually starts as intense itching and burning of the skin on the hand and fingers (and sometimes the soles of the feet), which can then erupt into small itchy blisters that may weep fluid

Eczema causes visible irritation and itching of the skin that can lead to sore and painful skin. Avoid scratching, or use emollients to help relieve and treat the pain.

Chronic scratching and rubing as result of eczema can result in thickened areas of skin. These areas of skin are always hyper-pigmented and always dry, scaly and leathery in appearance.

Eczema triggers can vary from person to person and depend on the type of eczema. Here are some of the most common:
Allergens cause a reaction in some people with eczema. This happens after you come into contact with a substance that has previously made you become sensitive to its effects. Common allergens include the house-dust mite, pollen, cosmetics, hair dyes, perfume, plants, medicines and metals such as the nickel and cobalt that you find in jewellery. Allergies often run in families.
How to avoid:
Almost half of people with eczema say clothing can irritate their eczema. This can include fabrics such as wool, silk and synthetic fibres.
How to avoid:
Soaps, detergents and fragrances can cause additional skin irritation for the majority of those with eczema.
How to avoid:
Around a third of people with eczema say what they eat, and drink is a trigger. Some foods can cause allergic reactions in people with atopic eczema, such as cow’s milk. Other foods can cause contact dermatitis, for example, citrus fruits, raw onions, garlic, tomatoes, peppers and chillies.
How to avoid:
Stress is a trigger for 9 out of 10 people with eczema. In response to fear or stress, your body produces cortisol which is released from the adrenal glands as part of the fight-or-flight response. This dampens the immune system and can cause an inflammatory reaction in our skin.
How to avoid:
Around 70% of people with eczema find the weather or temperature can trigger symptoms. You might find your symptoms are better in the summer than in the winter as central heating can dry out your skin. However, sweating in hot weather can also irritate your skin.
How to avoid:
As well as avoiding triggers that can make your eczema flare-up, there are many different ways you can manage your eczema.
Emollients are moisturizers that can help with dryness and itching. They can come in many forms including creams, lotions, ointments or sprays. Emollients should be applied to the skin regularly, sometimes even multiple times a day. The area of coverage and frequency will change depending on your symptoms and condition, the severity and which product you are using. Always refer to the label for proper use. Having well moisturised skin can help create a barrier which can prevent flare-ups.
Itchiness is a common eczema symptom, so finding a way to manage this itch is important. In fact, some emollients contain extra ingredients to help control itchiness. Ingredients such as oatmeal have anti-itch properties, or lauromacrogols, which relieve itch through a local anaesthetic action.
As regular soaps and cleansers can irritate the skin and cause dryness, it’s also important to consider washing with an emollient too. There are special emollients that can be used for washing just as you would use soap, or you can apply your leave-on emollient as a soap substitute. Be prepared though – while emollient soap substitutes clean effectively, they don’t lather up like regular soap. You can also add emollients to your bath.
Mild steroids creams and ointments can be bought from your pharmacy to help relieve contact dermatitis and mild-to-moderate eczema. These help manage flare-ups in atopic eczema by altering the body’s responses to inflammatory reactions. Always check the label for how to use the product correctly and safely; always check who can use the product as many over the counter steroids having limitations regarding age and pregnancy.
Always carry on using your emollient alongside your steroid but leave about 20-30 minutes between applying each one. If it’s the first time you have used a steroid cream – as with any new medicine – speak to your pharmacist or doctor first to find out if it’s the right choice for you. They will also be able to give you tips on how to apply correctly.
If you find that using a mild steroid cream for a week doesn’t bring your eczema under control, see your doctor. They’ll be able to prescribe stronger steroids that may be more effective for you.
Antihistamines can be used to help relieve severe itch in atopic eczema and contact dermatitis. Although they are available in a number of different formats (such as tablets, capsules, syrups or creams), tablets or syrups are most likely to be recommended. Non-drowsy antihistamines, such as cetirizine or loratadine, are recommended if you have atopic eczema with severe itch or urticaria. Ask your pharmacist or doctor for advice on taking an antihistamine that is right for you. If these do not work, or if you are using antihistamines for a prolonged amount of time, please go and talk to your doctor for guidance.